More than three months since the first registered cases of COVID-19 appeared in Kazakhstan, the epidemic continues to worsen in the country. Neither an effective treatment nor a vaccine for the novel coronavirus yet exist, hospitals across the country are overwhelmed, and every day new cases are reported. All of this is inevitably anxiety-inducing. We once again turned to the experts from the Association of Kazakhstan Family Physicians and asked them to answer the most popular questions people are asking these days. The AKFP doctors explained, as adepts of evidence-based medicine, what to do if you suspect you have coronavirus, why you don’t need to run to get tested, what hospitals are using to treat COVID-19 patients, who really needs to go to the hospital, and more.
You can read Adamdar/CA and AKFP's first collaborative article on the COVID-19 virus and prevention measures from March 19 at this link.
The information presented below was up-to-date at the time of publication, July 1, 2020.
IF YOU’RE SICK
I have symptoms of a coronavirus infection / I suspect that I have coronavirus / I have tested positive for coronavirus / A CT scan showed that I have signs of viral pneumonia. What should I do?
Your next steps depend on your condition and symptoms.
Remember that 80% of those who contract COVID-19 either do not exhibit any symptoms or have mild symptoms.
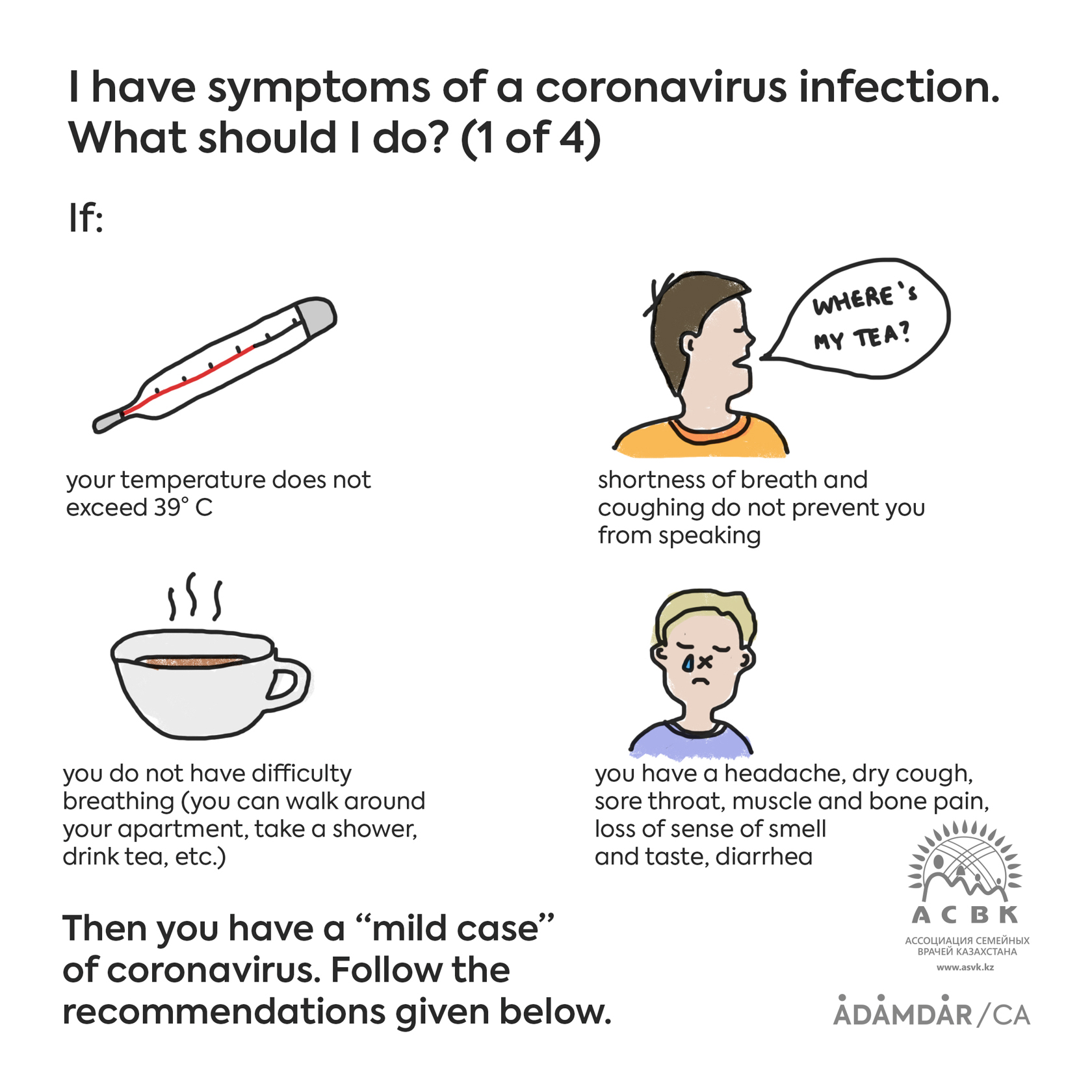
Mild symptoms of a coronavirus infection are:
• your body temperature does not exceed 39° C
• you do not have difficulty breathing (you can walk around your apartment/house, take a shower, go to the bathroom, drink tea, etc.)
• shortness of breath and coughing do not prevent you from speaking
• you may or may not have other symptoms—headache, dry cough, sore throat, muscle and bone pain, loss of sense of smell and taste, and/or diarrhea
If mild symptoms develop, follow the general guidelines below:
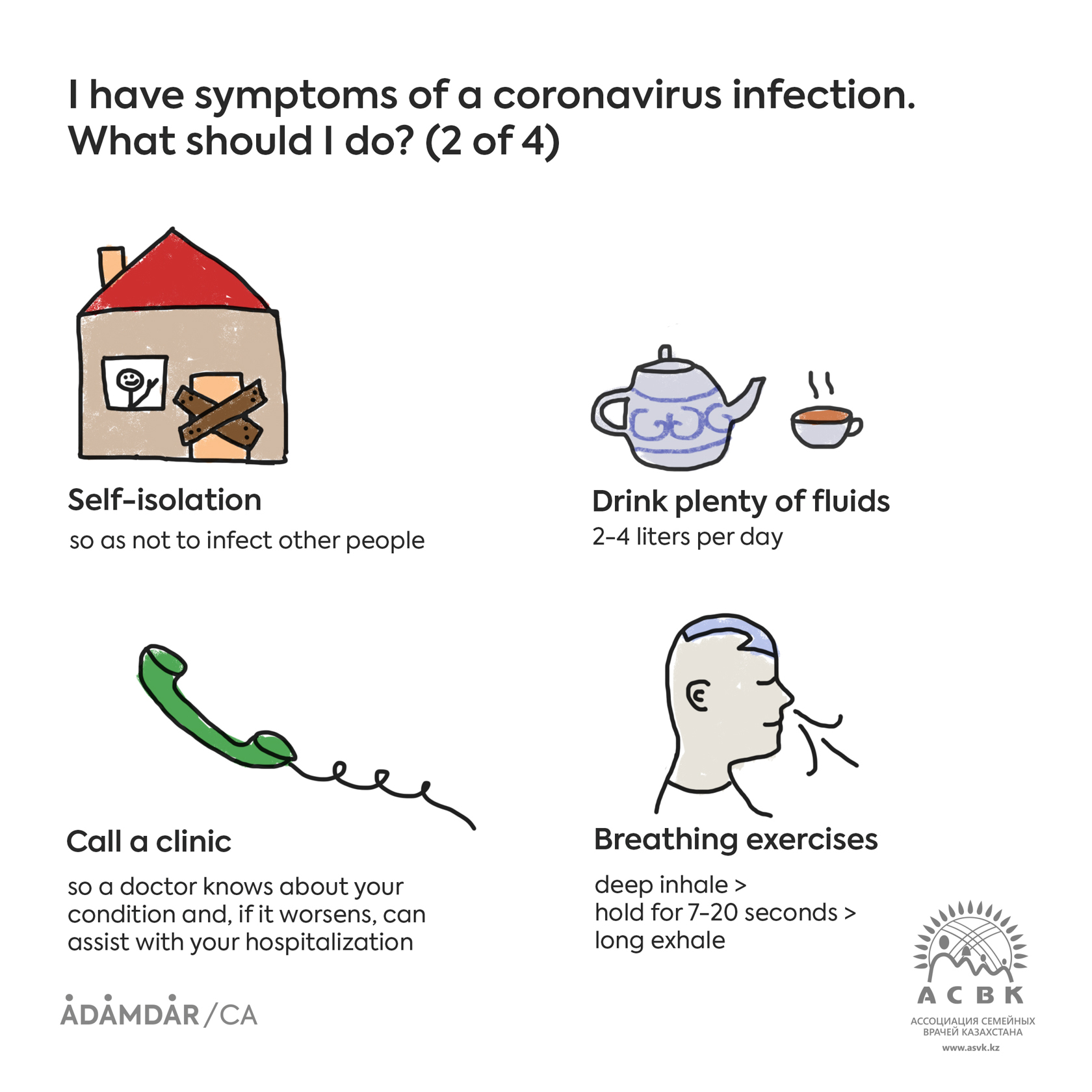
1) Self-isolation—so as not to infect other people
Stay home. If you do not live alone, you should have a separate room, and the door should always be closed. The room itself should be constantly ventilated, and all surfaces should be regularly treated with disinfectants. Members of your family should leave all your necessities (food, drinks, hygiene products, etc.) outside your door. If you leave your room to use the bathroom, you need to wear a mask, sanitize all surfaces you have touched with a disinfectant, and also meticulously wash your hands with soap and use hand sanitizer (alcohol solution).
2) Call a clinic and tell а general practitioner about your symptoms
It’s necessary for a doctor to monitor your symptoms remotely and, if they worsen, assist with your hospitalization.
3) Drink plenty of warm fluids—2-4 liters per day
Increasing your fluid intake helps to reduce toxins, alleviate headache and fever, overcome dehydration (fever, shortness of breath, and nausea cause your body to lose a lot of fluid), and dilute the blood.
What to drink? Primarily, clean water (2-3 liters), any kind of tea with raspberry, currants, sea buckthorn, barberry, or honey (if you’re not allergic), and broth (chicken, beef, mutton). It’s not advisable to drink a lot of sugary beverages, especially for people who are overweight.
4) Breathing exercises—2-3 times per day
Breathing exercises prevent stagnation in the lungs and increase lung capacity. The basic principle is to hold your breath for 7-20 seconds after a deep inhale. Then, a strong, extended exhale. You need to engage the lower rear sections of the lungs. Try not to lounge around in bed or sit for too long.
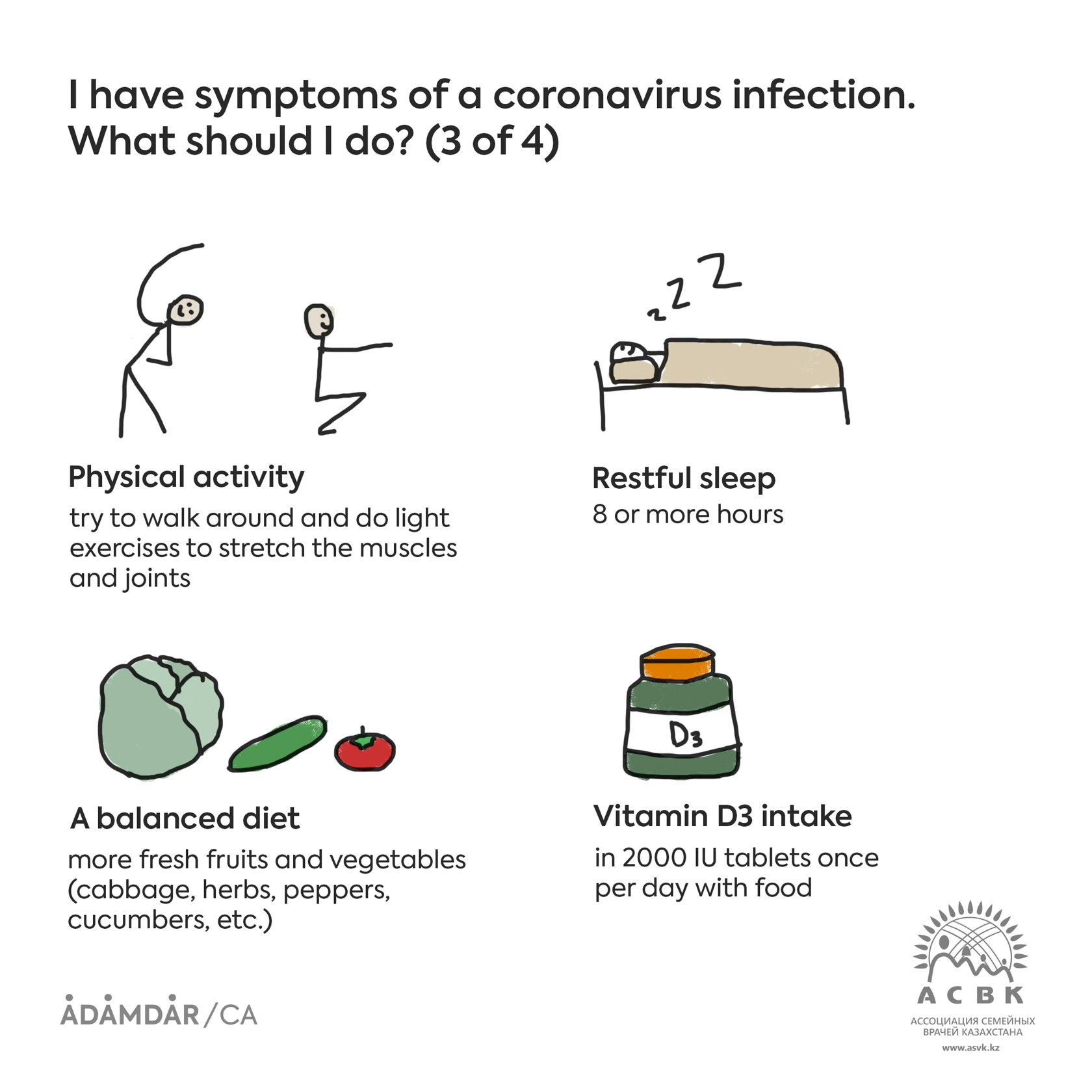
5) Physical activity
Try to get up, walk around, and do light exercises to stretch the muscles and joints: twists, bends, etc. Even if you feel weak, do not lie for too long on your back; turn onto your side or stomach frequently.
6) Restful sleep
At least 8 hours per day.
7) A balanced diet
Try to eat more fresh fruits and vegetables (cabbage, herbs, peppers, cucumbers, etc.).
8) Vitamin D3 intake
Vitamin D3 has been proven effective against other severe viral infections. Research has shown that a low level of vitamin D3 in the blood is linked to a more severe case of COVID-19. Take 2000 international units (IU) once per day with food, especially if you know that you have low D3.
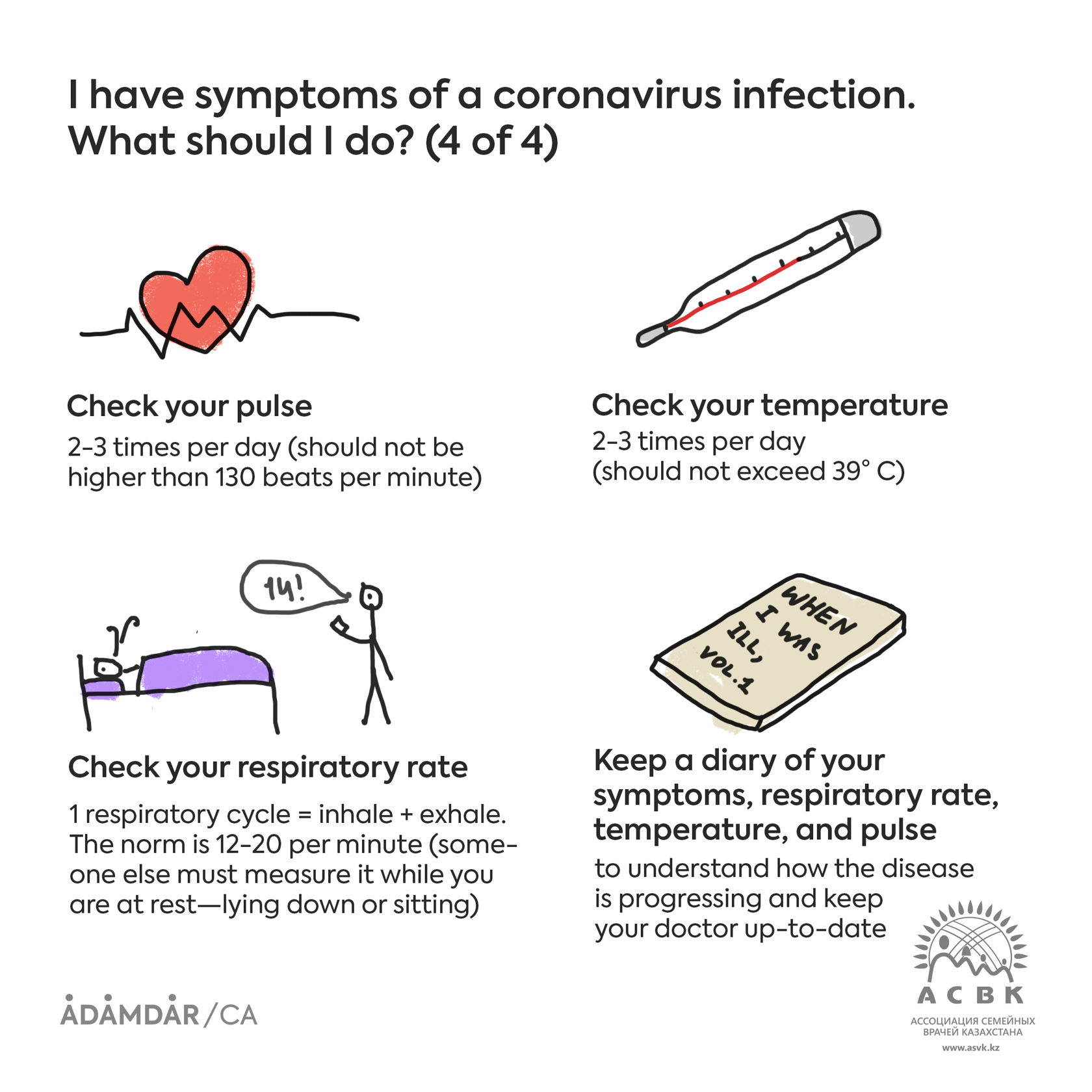
9) Check your respiratory rate per minute
One respiratory cycle is an inhale + exhale. Another person must measure your respiratory rate when you are relaxed, that is, sitting or lying down. A normal respiratory rate for an adult is between 12 and 20 cycles per minute, and a rate higher than 24 per minute is an indication of dyspnea (shortness of breath).
10) Check your temperature—2-3 times per day
11) Check your pulse—2-3 times per day
12) Symptom diary
Get a notebook in which to write down your symptoms, as well as your respiratory rate, temperature, and pulse. Relay these metrics to your physician. The Ministry of Health of the Republic of Kazakhstan has released a convenient checklist. You can download or view it here.
A treatment specifically for COVID-19 does not currently exist, so, if necessary, symptomatic treatment is recommended:
If you exhibit a severe fever or malaise (muscle pains, headache, aches in the body and joints, general malaise) regardless of temperature, you may take paracetamol or ibuprofen, but no more than three times per day.
For pain, sore throat, and cough, you can dissolve special antiseptic tablets, pills, lozenges, or lollipops in the mouth.
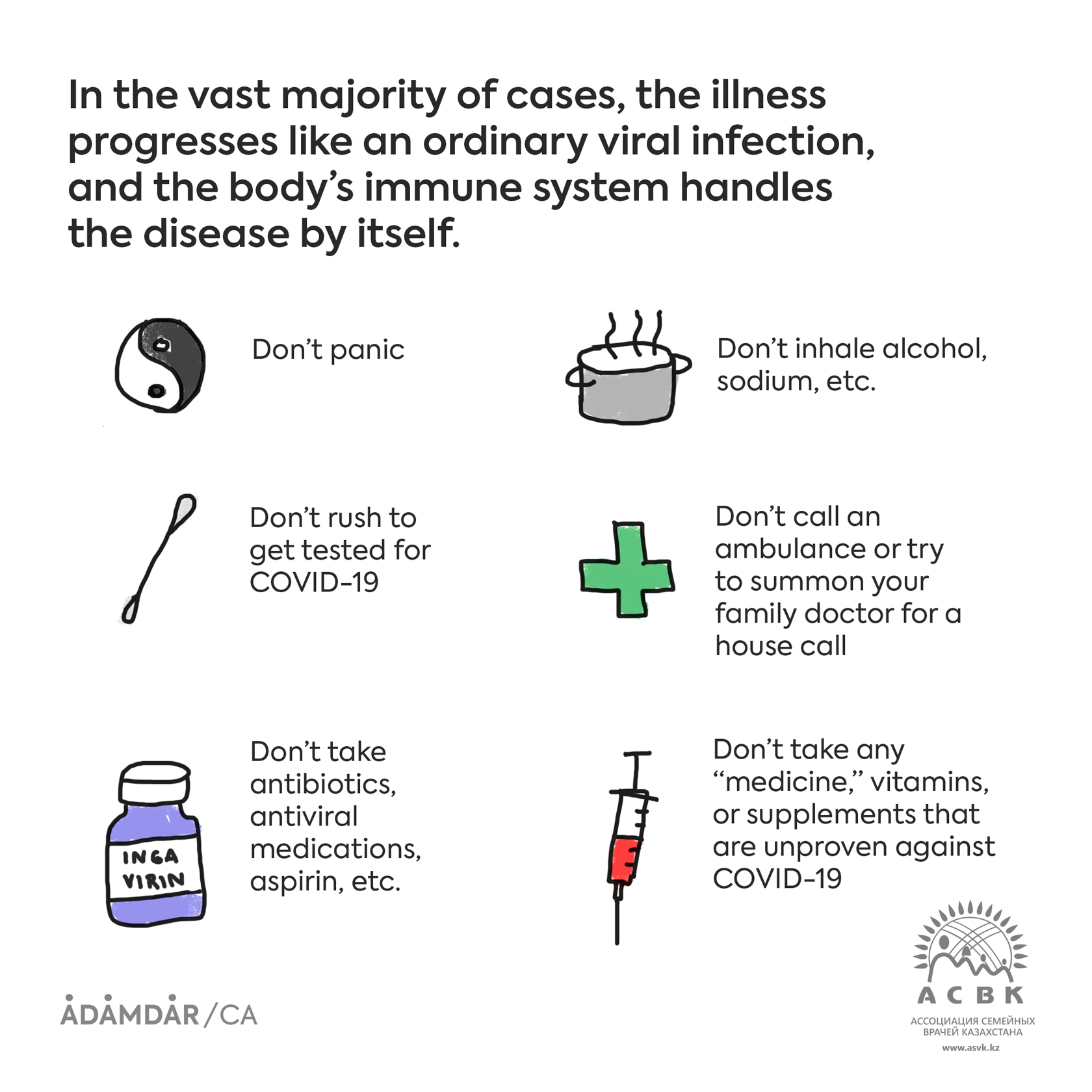
In the vast majority of cases, the illness progresses like an ordinary viral infection, and the body’s immune system handles the disease by itself. So:
• don’t panic
• don’t take any other, unproven “medicine,” vitamins, or supplements being pushed by dishonest manufacturers
• don’t inhale alcohol, sodium, or anything similar
• don’t call an ambulance or try to summon your family doctor for a house call unless absolutely necessary
• don’t take antibiotics, antiviral medications, aspirin, etc.
• there’s no need to rush to get a COVID-19 test
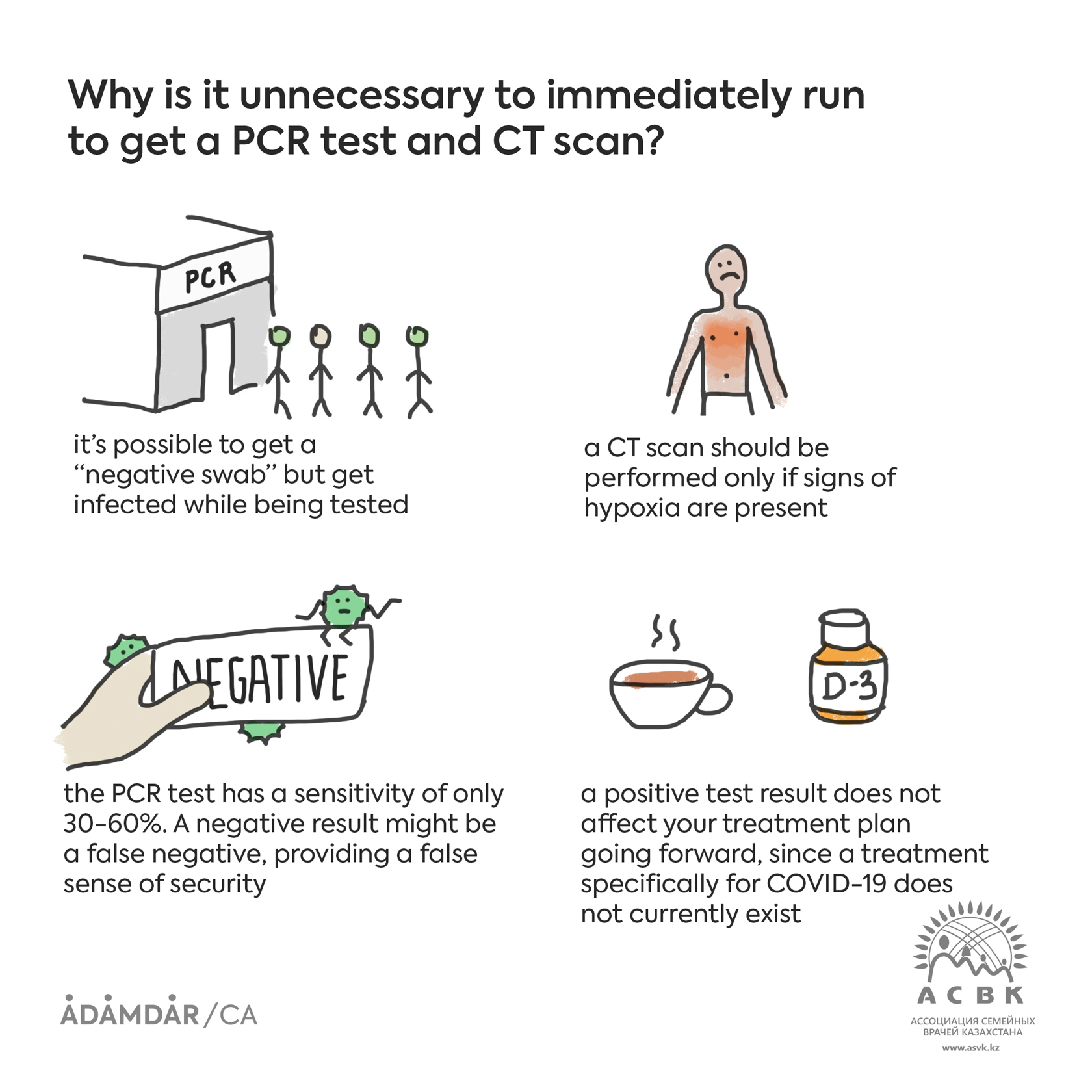
Why is it unnecessary to immediately run to get a PCR test and CT scan?
A coronavirus test won’t do any good if you don’t have symptoms. You can get a negative result from a nasal swab today but get infected tomorrow.
But even if you have symptoms, you don’t need to undertake any actions to make sure they are related to a coronavirus infection. These screening methods, unfortunately, don’t give any concrete answers to the questions of what to do next, how to get better, or what to take. The sensitivity of a PCR (Polymerase Chain Reaction) test is not high (30-60%) and depends on a variety of factors. If you have symptoms typical of the disease but a “negative swab,” you are most likely infected with coronavirus nonetheless.
A test does not impact your chance of recovery in any way, but it may seriously complicate your situation. For example, you may get infected while getting tested. Any visit to a hospital, clinic, or laboratory carries the danger of infection because sick people frequent those places. A negative test result creates a false sense of security, since COVID-19 tests frequently give false negatives. A positive test result does not affect your treatment plan either, since a treatment specifically for coronavirus infections does not currently exist, and, in any case, the outcome depends on your immune system.
A computerized tomography (CT) scan of the lungs is used not to detect coronavirus, but to diagnose viral pneumonia. As with the PCR test, detecting disease indicators with a CT scan, even bilateral pneumonia, in and of itself does not affect what needs to be done next. CT scans of even the most mildly affected COVID-19 patients sometimes identify bilateral pneumonia that resolves itself in the long term. Furthermore, the scanners are often not properly disinfected, so even if you do not have COVID-19, you may be infected with it in the scanner, in the waiting area, or while interacting with staff. A CT scan should be performed only in the event that the patient’s condition is sufficiently severe and hospitalization is being considered, or if the patient shows signs of hypoxia, i.e., oxygen starvation.
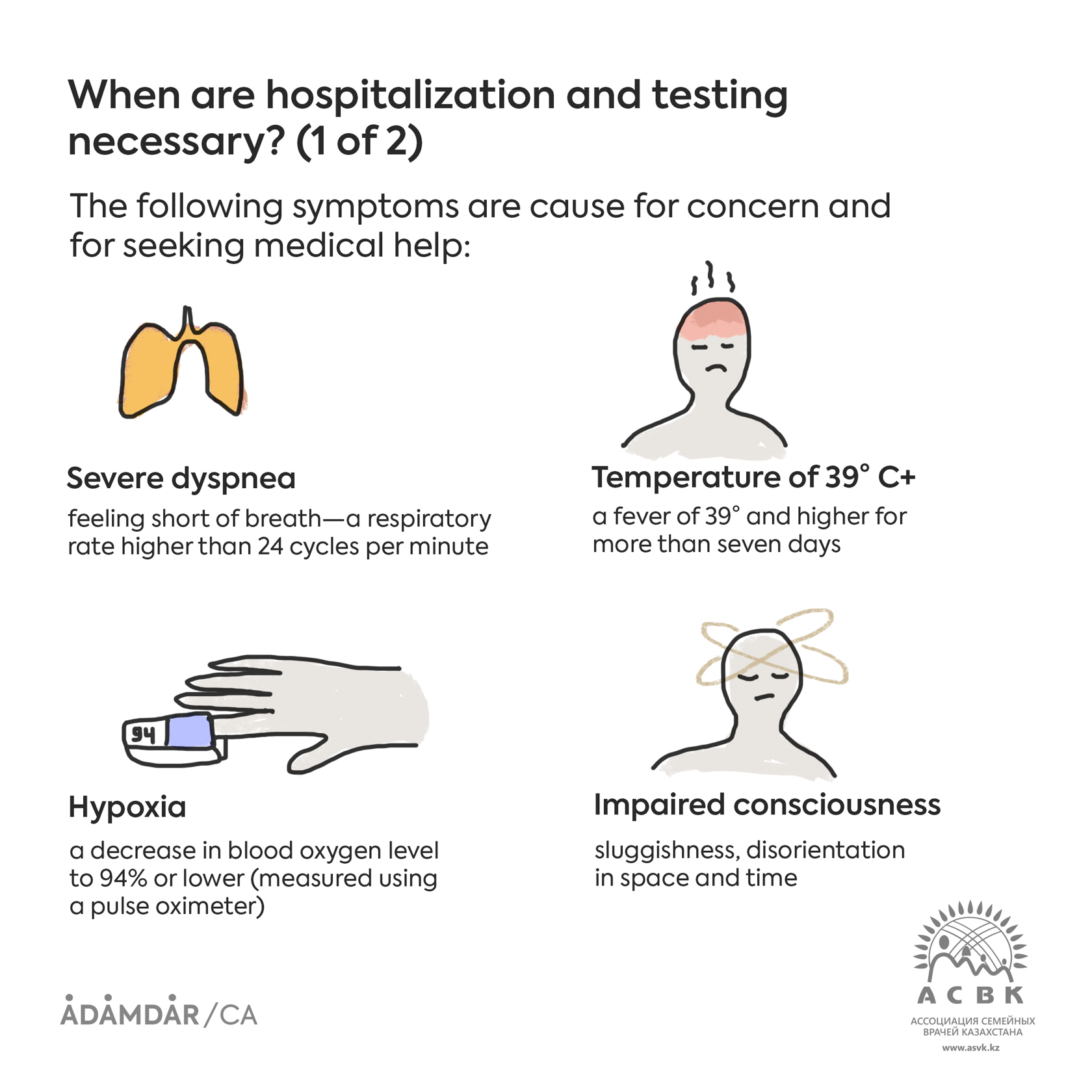
When are hospitalization and testing necessary?
Hospitalization and testing for coronavirus (PMR, CT scans of the lungs) are needed only for the severely ill when oxygen support or treatment in the ICU are on the table. Only 20% of those infected require hospital care.
The following symptoms are cause for concern and for seeking medical help:
1) Severe dyspnea* (shortness of breath)
a respiratory rate higher than 24 cycles per minute
*Dyspnea is classified according to severity:
Mild: shortness of breath that does not interfere with daily tasks (may affect you when climbing 1-2 flights of stairs or walking briskly)
Moderate: shortness of breath that restricts your everyday life (e.g. you have to pause to rest while climbing stairs, or your shortness of breath bothers you while cooking and doing light housework)
Severe: shortness of breath that occurs while you are at rest, leaves you unable to speak in complete sentences, and interferes with simple tasks, like bathing or getting dressed.
2) High temperature
A fever of 39°C or higher that does not go down after taking antipyretics and persists for an extended period of time (more than seven days).
3) Decrease in blood oxygen level
Blood oxygen saturation is measured using a pulse oximeter—a small device that is attached to the pointer or index finger. It shows the level of blood oxygen as a percentile. A 94% blood oxygen level or lower is a sign that the lungs are not functioning properly and the patient needs oxygen support.
4) Impaired consciousness
sluggishness, disorientation in space and time
5) Decrease or sharp increase in blood pressure
less than 90 mmHg or 220 mmHg and higher
6) Elevated pulse
higher than 130 beats per minute
7) Presence of additional risk factors
age 65+, accompanying cardiovascular disease, diabetes, obesity, cancer, et al.
8) Other severe symptoms
for example, intolerable pain (in particular, headache), uncontrollable vomiting, or persistent diarrhea
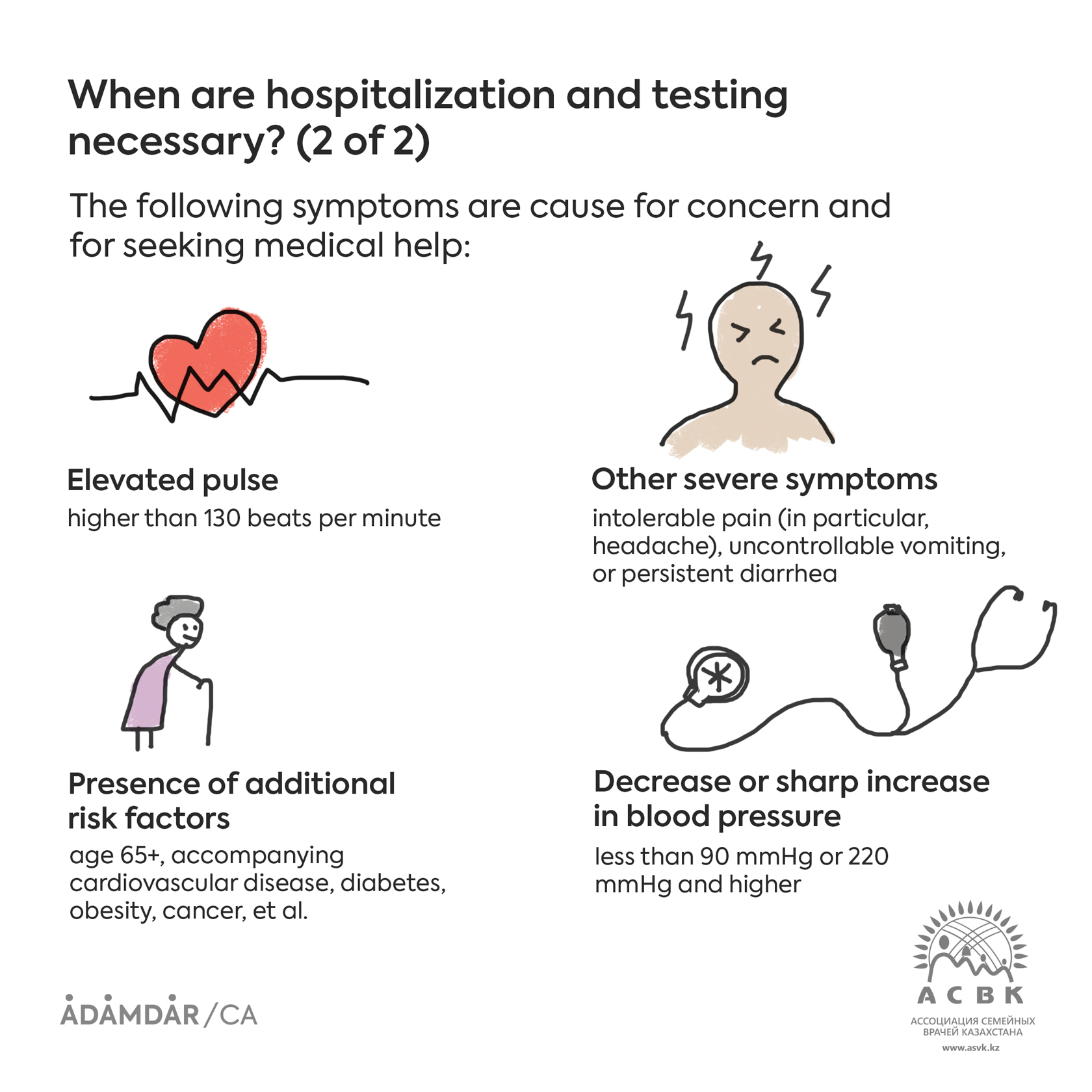
* A combination of two or more of these symptoms indicates a need for hospitalization. You should inform your clinic’s GP (general practitioner) of your condition or call an ambulance.
Seeking medical help to keep your condition from worsening and prevent complications, which is something we always do with other illnesses, unfortunately does not work for coronavirus. Medical personnel cannot help you in this way, as the course of the disease and its outcome depends solely on your immune system. Moreover, not only does unnecessary contact with medical personnel without good reason not provide any benefit, but it also carries the risk that you will get coronavirus there if you only had a regular viral or bacterial infection before.
I tested negative for COVID-19, but a CT scan showed bilateral pneumonia. How is this possible?
The accuracy of a COVID-19 test is highly dependent on the correctness of the nasal swab. Not all medical personnel can correctly collect a sample from the posterior wall of the pharynx. The result also depends on the quality of the PCR diagnostic.
CT results are far more informative. If you have COVID-19, the images will immediately show a typical picture, and the diagnosis is practically obvious. PCR tests are important for statistics, but do not play an important role in determining treatment.
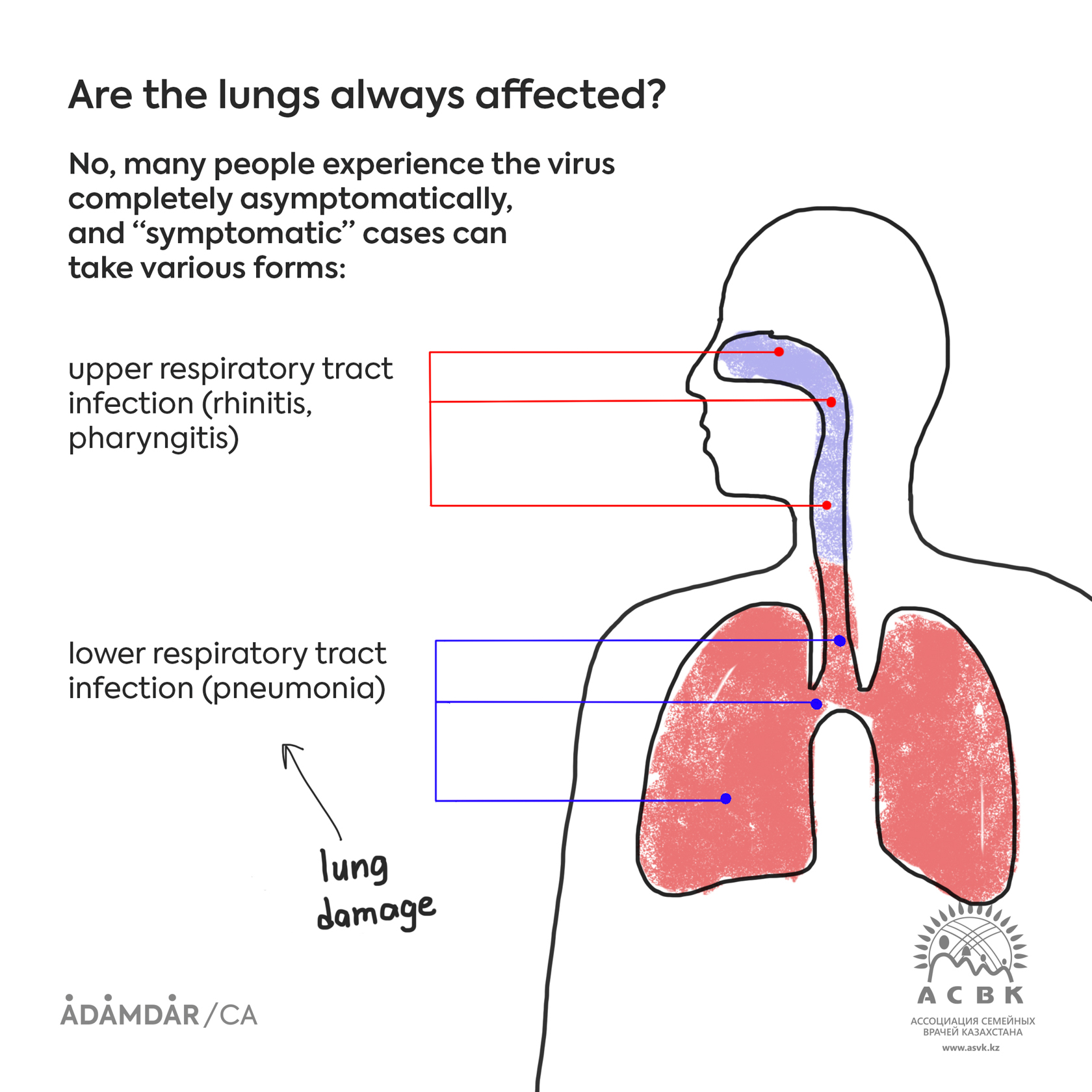
Are the lungs always affected?
A coronavirus infection can take many forms and does not always cause lung damage. Often, the disease runs its course completely asymptomatically.
In symptomatic cases the disease is divided into the following types:
• coronavirus infection impacting the upper respiratory tract (rhinitis, pharyngitis)
• coronavirus infection impacting the lower respiratory tract (pneumonia)
Lung damage has only been observed in the latter. Thus, the disease progresses without lung damage for the majority of patients.
I’m sick and have small children. I can’t isolate myself from them. What should I do?
It’s practically impossible to avoid infection when you’re in close contact with children. If it’s impossible for you to self-isolate, expect that your children will also catch it because the virus is highly contagious. Even constant protection measures—handwashing with soap, masks, sanitizers, saline solutions—will not be enough to prevent the transmission of the infection in close quarters.
But at the same time, you should know that children generally experience COVID-19 asymptomatically or in a mild form. Symptoms such as runny nose, moderate fever, sore throat, and loose stool may develop, but in most cases, children feel fine and do not experience, compared to adults, malaise, weakness, or lack of appetite. If symptoms develop, symptomatic treatment should be followed: swaddle the child, flush their nose with saline solution, and for a fever higher than 38.5° С, give them children’s paracetamol.
According to research, newborns and teenagers are at risk. Scientists are still developing theories, so there are no definite explanations yet.
What is being used for treatment in hospitals?
In hospitals there is not a particular treatment, as there are no medicines that have been proven effective and safe against COVID-19.
The hospital can help you deal with complications of COVID-19: primarily, respiratory distress, which is expressed by lowered oxygen levels in the body and is manifested by severe shortness of breath. Breathing problems arise if the virus has penetrated the lungs and caused pneumonia. Severe shortness of breath prevents the person from walking, or even sitting and speaking.
Blood oxygen level can be determined using a pulse oximeter. EMTs, hospital doctors, and some general physicians have these devices. Blood oxygen lower than 94% in an adult, as well as a respiratory rate of more than 24 cycles per minute, indicates the need for hospitalization and oxygen inhalation through nasal tubes (cannulas).
IVs help reduce dehydration, provide parenteral nutrition, and administer some medication to severely ill patients who are unable to drink. In hospitals, antibiotics are administered intravenously and antiviral medications are given in pill form.
If oxygen therapy doesn’t help, doctors turn to artificial respiration. Approximately 5% of those infected need intubation. The prognosis is poor for this group (mortality is about 80%). Also, blood clots increase in severe patients. Clots are treated with special medicines, called direct oral anticoagulants. Severe patients who have developed acute respiratory distress syndrome (ARDS) and a “cytokine storm” are also given immunosuppressants like dexamethasone in pill form or intravenously. Some countries have monoclonal antibodies in their ARDS treatment arsenal.
RECOVERY, RE-INFECTION, AFTERCARE
If someone is already ill with COVID-19 and is on the mend, do they need to be isolated from another sick person?
If you have coronavirus, then it’s necessary to cease contact with everyone who does not have the virus for two weeks. You cannot go outside or to the store, or socialize, whether it’s with relatives, loved ones, children, or the elderly.
If a family member or someone close to you also has coronavirus at the same time, then you may interact with each other. If this person gets the virus later, and you have already recovered after getting sick a week or two (or more) earlier, then it’s inadvisable for you to have contact with the “freshly” infected person.
Can recovered patients fall ill again?
The body produces antibodies in response to an infection. Antibodies are proteins that help fight infections and usually provide defense (immunity) against a recurrence. Antibodies are specific to the disease. For example, measles antibodies protect a person who has had contact with someone with measles but will not act if the person is infected with the flu.
COVID-19 is a new infection. Antibodies are being produced in response to this virus, too. But how resistant they are, whether they can prevent re-infection, and for how long is not yet known for sure. Therefore, we don’t have reliable data about whether a recurrence is possible. This question is currently being studied.
I think I had COVID-19 in the spring. Do I need to get a blood test for antibodies?
If you had the aforementioned symptoms, it’s possible that you had a coronavirus infection. Testing your blood for antibodies doesn’t make any difference. First of all, the sensitivity and specificity of these tests has not been sufficiently studied, so it’s unknown how precise they are in confirming that you came into contact with coronavirus. Therefore, detecting coronavirus antibodies in your blood does not guarantee total defense against re-infection. Rather, at the present you should be taking all infection prevention measures—just like everyone else around you.
How should patients be treated following recovery from coronavirus?
Unfortunately, too little time has passed to draw conclusions about the long-term impact of the virus. As of today we know that the consequences can manifest in various forms. This includes pulmonary fibrosis, myocarditis, and other inflammatory disorders. Breathing exercises are recommended in order to rehabilitate the respiratory system.
Inflating balloons is often recommended as a breathing exercise. Is this beneficial for COVID-19 patients?
Inflating balloons is an exercise of the respiratory muscles with increased exhalation resistance. This is beneficial for asthma and COPD (chronic obstructive pulmonary disease), as it teaches patients to lengthen their exhales. These diseases cause the bronchial lumen to contract.
This exercise is not necessary for COVID-19 patients; in this case it’s more important to work on the inhale because it’s not the bronchi that are affected but the alveoli. The respiratory surface decreases, and gas exchange is affected. While doing breathing exercises, it’s as if we expand this gas exchange surface and stop inflammatory fluid from filling the alveoli.
POPULAR MEDICATIONS AND TREATMENT METHODS
A lot of people are talking about the benefits of anticoagulants for COVID-19 patients. Should I take them as a preventative measure?
It's not necessary. Anticoagulants neither prevent nor treat the infection itself. They can help if complications develop in the form of blood clots. Increased clotting due to a virus penetrating the arteries and veins is extremely rare, and, furthermore, only occurs in the seriously ill, especially those in intensive care. Very “serious” drug injections are used to treat it, drugs like heparin and its derivatives. These drugs require monitoring of the coagulation system for a variety of indicators.
Are the popular medications that people have started stocking up on effective in the fight against COVID-19?
Medications like Nobazit (enisamium iodide), Ingavirin (pentanedioic acid imidazolyl ethanamide), and Interferon (human leukocyte interferon, powder to make a solution, or as a solution) have not been proven effective. All these medications are labeled as antiviral, but they have not gone through randomized clinical trials and are not used in countries that adhere to evidence-based medicine.
We advise you to view phrases like “immunomodulatory effect,” “immunity-boosting,” or “protector” on medicine instruction labels as a “red flag.” These very unscientific and vague concepts are often used by manufacturers of medications and supplements that have not been proven effective.
Tamiflu (oseltamivir), Relenza (zanamavir), and Inavir (laninamivir) only work against the flu (flu season is in the winter), but many people are now mistakenly taking these drugs against coronavirus.
Nimesil is the commercial name for nimesulide, one of dozens of non-steroid anti-inflammatory medications, a category which also includes aspirin, ibuprofen, Paracetamol (acetaminophen), diclofenac, and others. You should not take nimesil if you suspect you have COVID-19, as it has not gone through clinical trials for safety. As of today, only two medications are approved to be taken for severe symptoms, such as muscle and bone pain and severe fever: Paracetamol (acetaminofen is its international generic name) and ibuprofen.
People with a coronavirus infection cannot take Sumamed (its international generic name is azithromycin), Ceftriaxone, or any other antibiotics, as in doing so you disrupt your microbiome (destroying the good microbes in your gut and nasopharynx) and promote resistance to antibiotics. No antibiotics are effective against viruses! They are not just unhelpful, but harmful during a viral infection. You will be given antibiotics only to prevent a secondary bacterial infection that may enter the lungs during intubation if you are severely ill with COVID-19 and on a ventilator in the ICU.
On WhatsApp a certain course of treatment for coronavirus is being spread around that prescribes immediately taking antibiotics and antiviral medications. Is this a good idea?
Don’t pay attention to chain messages with courses of treatment for coronavirus, or any other sources of information advising you to take an antiviral or antibiotic something or other.
Unfortunately, as of today there is no specific treatment for coronavirus infections. This means that there is not a single drug with proven effectiveness that could arrest the development of the virus or stop the course of the disease and bring about a faster recovery. Therefore, there is no need to take antiviral medications or antibiotics in the first days of infection. There will definitely be no benefit to doing this, but the side effects of these medications are real and may worsen your condition and the course of the disease.
Antiviral and antibiotic drugs are prescribed for a secondary bacterial infection by a doctor. This carries major consequences, which the doctor monitors when treating severely ill patients in a hospital. And even in these cases, the treatment more often is of an empirical (experimental) nature, and there is no guarantee that the medications will work in any particular case.
Is it true that ibuprofen can cause complications?
In the beginning of the pandemic, it’s true that articles were published stating that COVID-19 patients who had taken ibuprofen were dying or experiencing complications at a higher rate. However, further investigation has fully exonerated ibuprofen.
Furthermore, it has been shown in randomized controlled experiments that ibuprofen, when taken for severe muscle pain, headache, or fever, is not only safe, but has an advantage over other similar drugs.

AKFP doctors are available for free online consultations through Telegram (languages: Russian/Kazakh).