What makes the COVID-19 virus different from other viruses? How can we strengthen our immune systems? Are cats and dogs dangerous in a pandemic? Can Adyraspan and lamb fat save us from Coronavirus? Where and how should we wear masks? Adamdar/CA asked these and many other important questions to experts from the Association of Kazakhstan Family Physicians.
The AKFP doctors provided us with detailed answers. We invite readers to study them carefully. Under the present circumstances, verified information can bolster health and save lives.
ABOUT THE VIRUS
What is COVID-19, how is it dangerous, and how is it different from other viruses that we have seen before (SARS, swine flu, etc.)?
COVID-19 is an infectious disease caused by a new, previously unknown virus — SARS-CoV-2 from the Coronavirus family. The virus was first identified in Wuhan, China in December 2019.
There are several key differences from previous known coronaviruses:
1. A longer incubation period: on average, about 5 days (for comparison, SARS’ is 1-2 days) and a milder course of the disease.
This allows sick people with mild symptoms of the common cold, which comprise 80% of cases, to infect a large number of people over a longer period. With SARS and swine flu, the symptoms developed so rapidly that people quickly realized that they were sick and immediately sought treatment.
2. There are two risk groups in which the virus can cause a more severe course of the disease and complications:
• persons over 60 years old
• people with chronic diseases regardless of age (diabetes, hypertension, asthma, autoimmune diseases, cardiovascular diseases, cancer, etc.)
According to statistics, about 15% of patients will have a moderate to severe case of the disease. That is, they will need treatment in a hospital. Another 5% of all patients will need life support. Given the fact that in hospitals, as a rule, there are not enough available ventilation machines, a sharp increase in the number of severe patients will overload the healthcare system of any country.
How is COVID-19 transmitted?
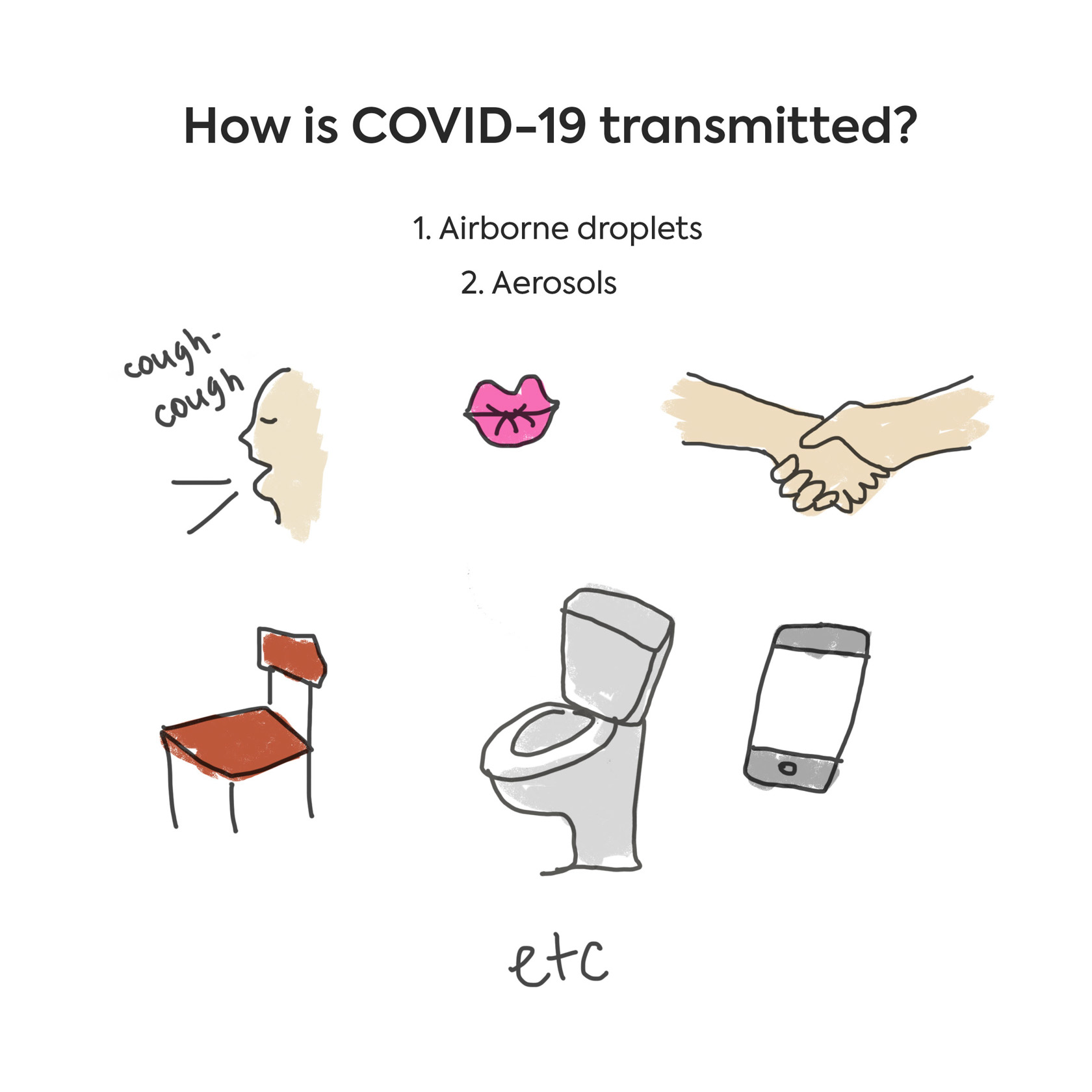
Coronavirus is transmitted from person to person in several ways:
Airborne droplets: Particles secreted by sneezing, coughing, kissing, shaking hands, and hugging are transferred to the face, eyes, and hands of a healthy person either by a sick individual or by a carrier (a person who does not experience symptoms, but who still has the virus on their mucus membranes).
An airborne droplet can travel 2-3 meters between people during direct communication. You can also get infected via droplets by touching objects that an infected individual has recently touched. Most often these objects are door handles, ATM buttons, elevators, cell phones, railings, counters, tables, chairs, glasses, cups, spoons, a computer keyboard, handrails and other such surfaces.
Aerosols: Dried out particles from the respiratory tract’s mucous membranes, together with viruses, can penetrate airflows into other rooms, especially if the rooms share a common ventilation system.
This is exactly what happened on the Grand Princess cruise ship. In addition to being excreted with saliva or mucus, the virus can also be transmitted via the feces and urine of the patient, though this mode of transmission is less common. When you flush the toilet, a tiny aerosol containing viruses is created. Aerosol flies much further than droplets. The virus may be able to reach a person living nearby an infected individual via sewer pipes. It is recommended to flush toilets with the lid closed and keep toilets closed when not in use.
Is it possible to get infected through products/goods or from animals?
It’s hypothetically possible. For example, if an infected waiter sneezed or coughed on plates or a drink that he immediately served to you. Or, if the same waiter gave you cutlery that he had touched with his unwashed hands. However, there is no direct evidence of this method of transmission.
There is a possible risk of infection if a person, either ill with or an asymptomatic carrier of COVID-19, touched merchandise on the shelves of a store, you handled these products and then, without washing your hands, touched your face or eyes.
If you received a package that has been left out for more than 12 hours, then any virus that might have been on it most likely has already died. Goods that you bring into your home should be picked up with gloves and wiped with alcohol. Handles, bags and boxes should be handled after sanitization.
There are no recorded instances of transmission of coronavirus through pets.
They say that children are not affected by this virus, is that so?
In children, the disease is asymptomatic, but they can be hidden vectors of COVID-19 infection and pose a potential danger to adults.
Specialists from a children's center in Guangzhou, China, tested 745 children aged two months to 15 years from families where coronavirus infections were detected. Infection was confirmed in ten of them. However, not a single infected child displayed the symptoms of COVID-19: fever, fever, muscle pain, weakness, shortness of breath, or pneumonia.
PREVENTION AND MASKS
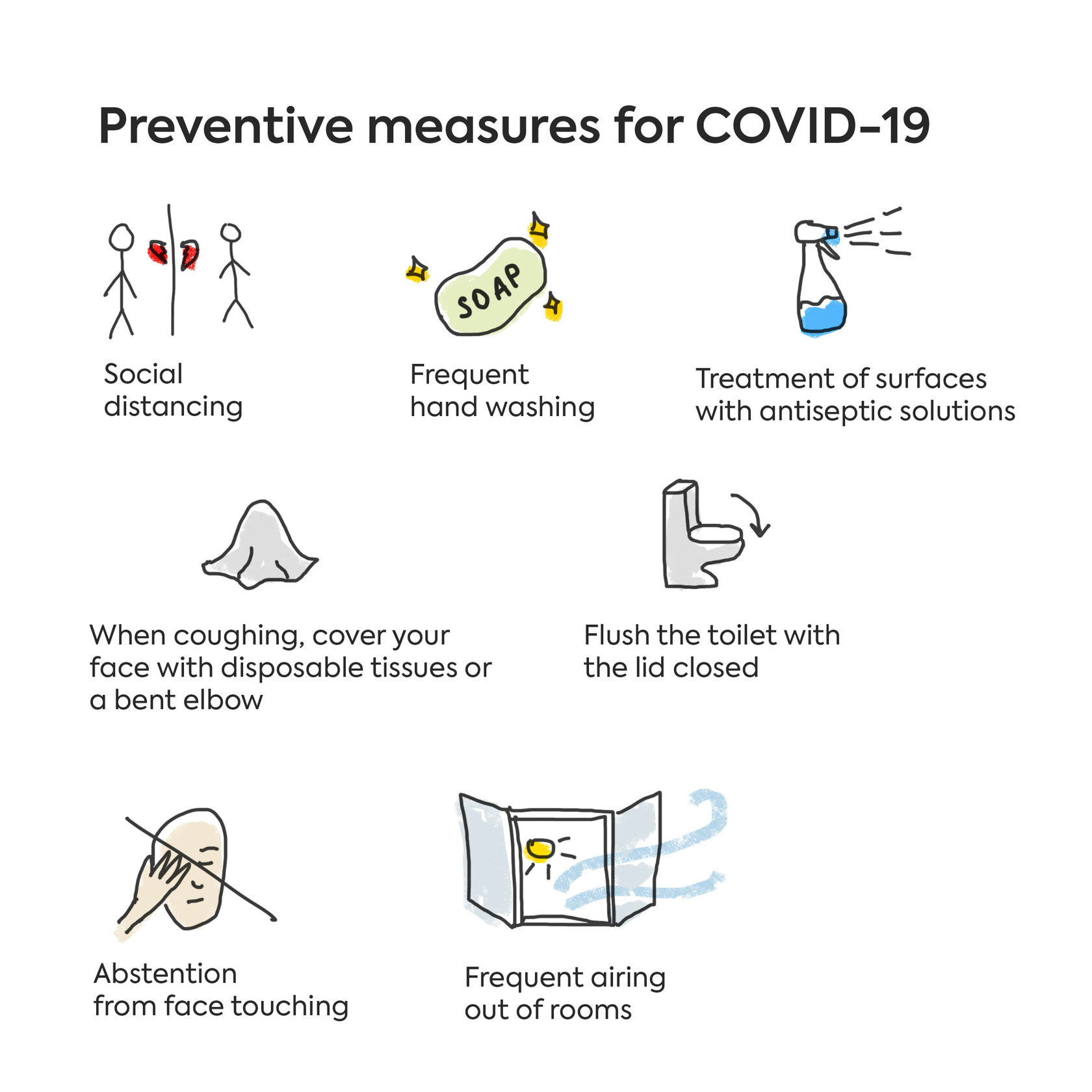
What are the main preventive measures for COVID-19?
• Social distancing (when possible, avoid crowded places, events, cinemas, theaters, shopping and entertainment centers, playgrounds, etc.)
• Frequent hand washing with warm water and soap (for at least 20 seconds) or application of alcohol-based hand sanitizer
• Frequent airing out of rooms
• Treatment of surfaces with antiseptic solutions
• Abstention from face touching
• When coughing and sneezing, cover your face with disposable tissues or sneeze into a bent elbow. After use, immediately throw away the tissue and wash your hands with soap and water or use a hand sanitizer.
• Flush the toilet with the lid closed
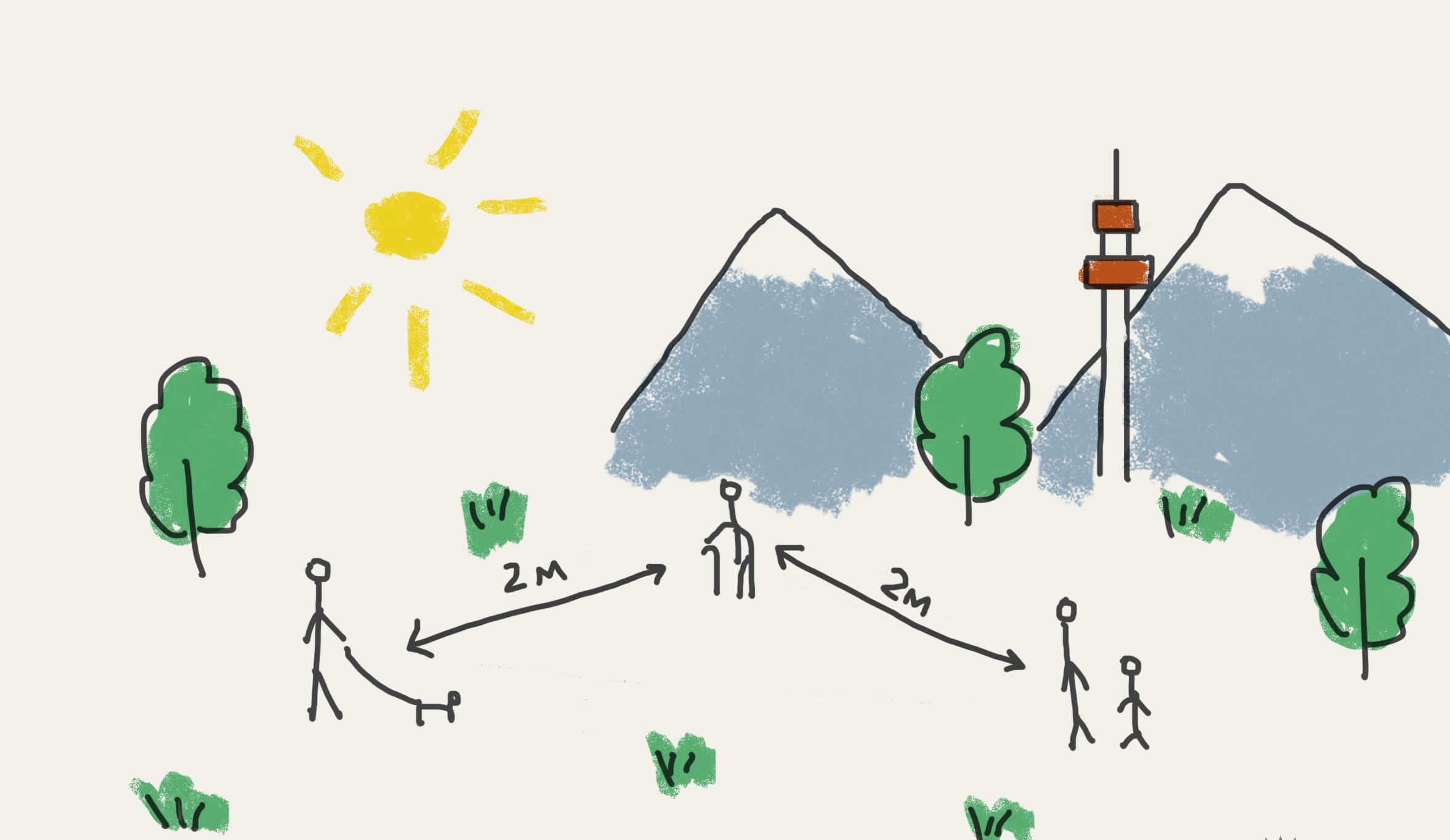
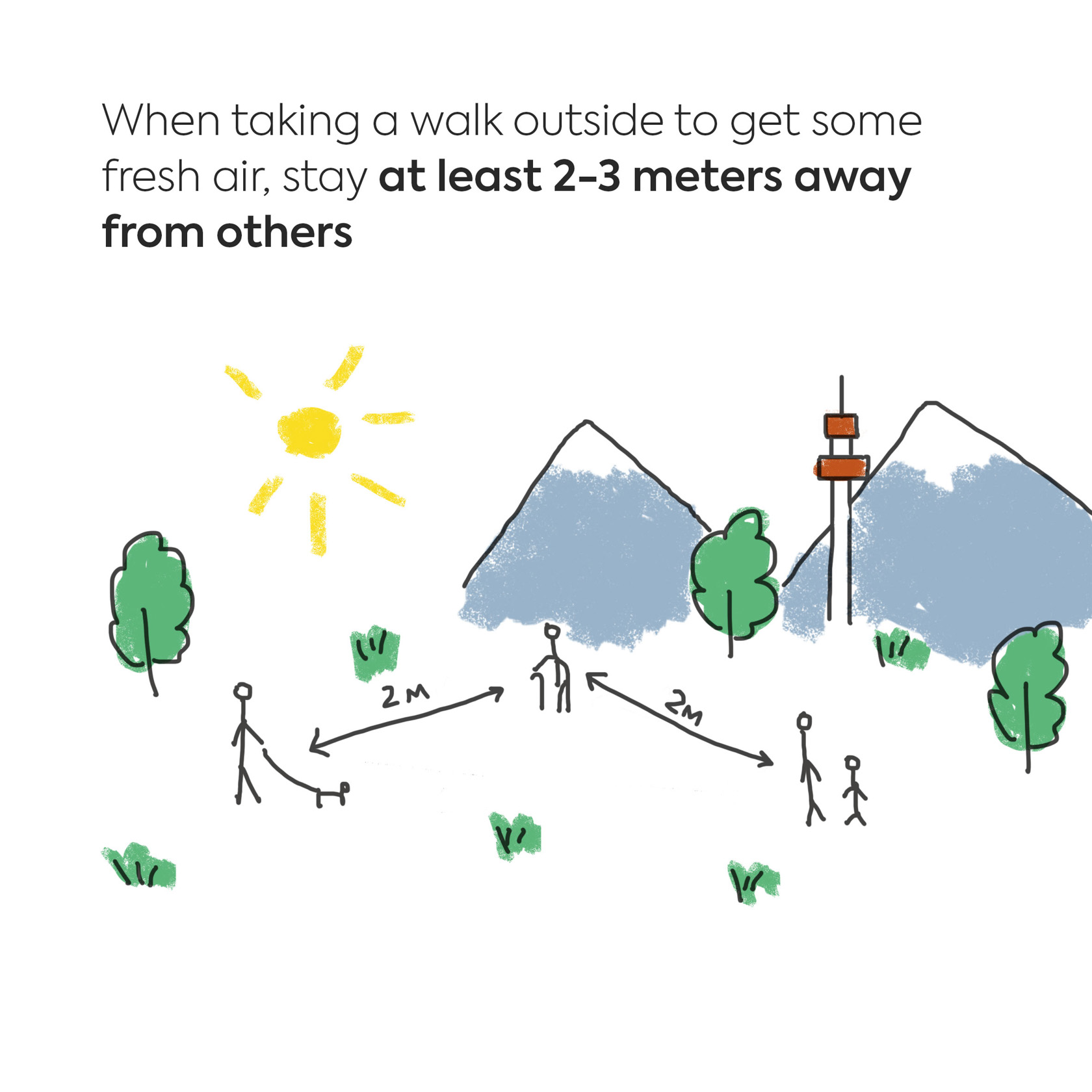
• When taking a walk outside to get some fresh air, stay at least 2-3 meters away from others. Visiting playgrounds and other attractions is not recommended.
When do you really need to wear a mask?
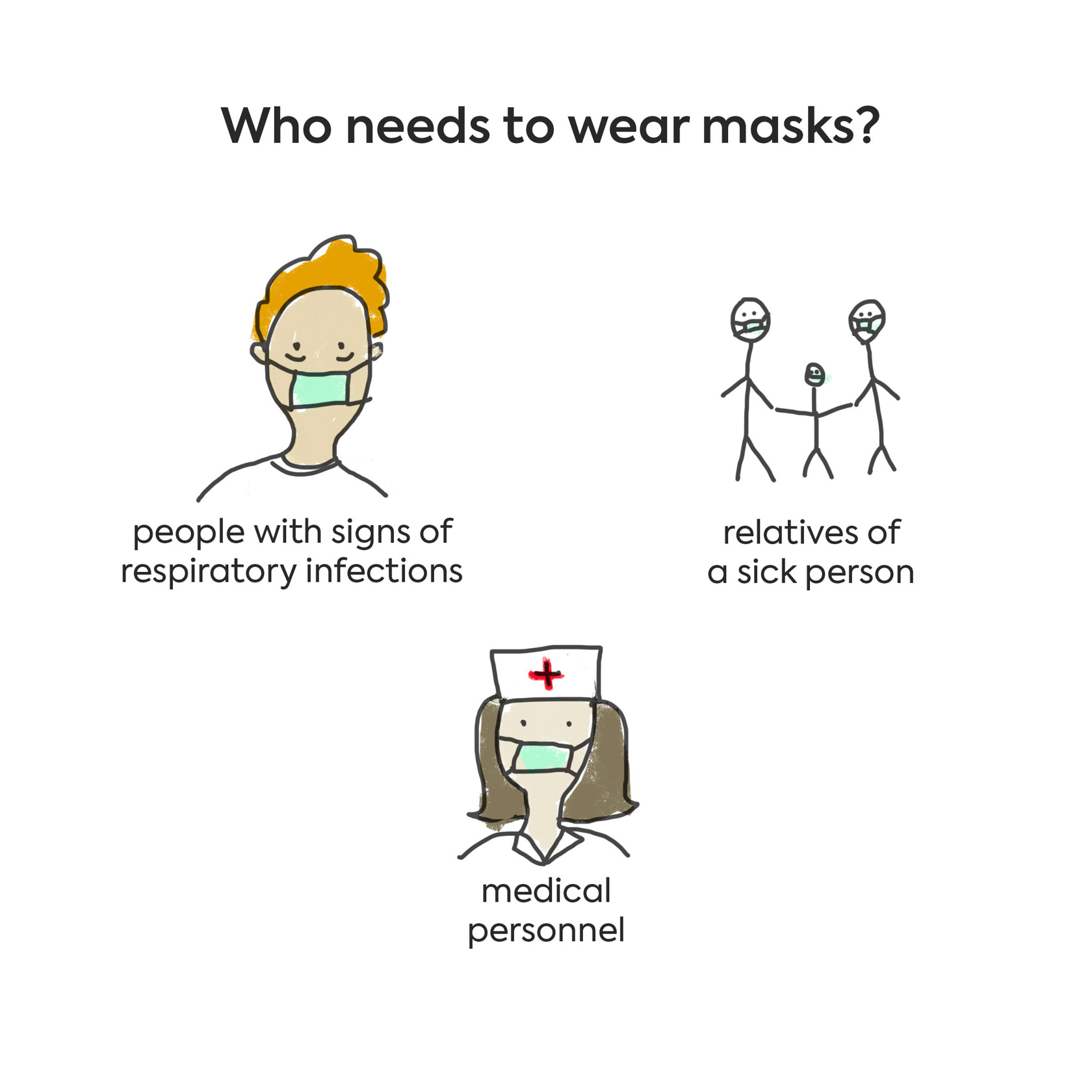
To reduce the risk of infection, the CDC and WHO recommend that masks should be worn by people with signs of respiratory infections (such as colds), relatives of a sick person, and medical personnel.
There is no conclusive evidence to point to any benefits of wearing masks by individuals without symptoms of the disease. Since mask shortages are currently widespread around the world, experts recommend leaving them for groups who need them the most.
How do you put on and take off a mask?
• Before putting on the mask, wash your hands with soap in accordance with all the rules (see below) or treat them with a sanitizer. Dry your hands with a napkin.
• Wear the mask in such a way that it covers both the mouth and nose. Make sure it fits the face tightly.
• When wearing a mask, be careful not to touch the fabric with your hands.
• Remove the mask using the rubber bands on the sides. Do not touch the front surface.
• Fold the used mask with the part adjacent to your face facing inward and throw it away.
• After changing masks, wash your hands or treat them with a sanitizer in accordance with the rules.
Change the mask as soon as it becomes damp (but at maximum, every 2 hours).

What do masks protect us from, and what are they ineffective against?
To some extent, conventional surgical masks help protect the people around an infected person from the larger droplets of saliva and mucus that they secrete when they cough and sneeze.
They do not protect healthy people from infection, as they do not create a snug, airtight seal on the face. If the rules for mask wearing are not followed, they can do more harm than good to healthy people.
DIAGNOSIS AND TREATMENT
What do you do if you suspect you have COVID-19?
1. Watch for symptoms
Stay home if you have symptoms of the coronavirus infection:
• Fever
This means that you feel an elevated temperature when touching your chest or back (it is not necessary to measure your temperature to recognize a fever).
• A persistent cough (recently developed)
Persistent means that you cough for more than an hour, or you have 3 or more episodes of coughing within 24 hours (if you usually have a chronic cough, it may become worse than usual).
If you experience this symptom, do not go to a general practitioner, clinic, pharmacy, or hospital.
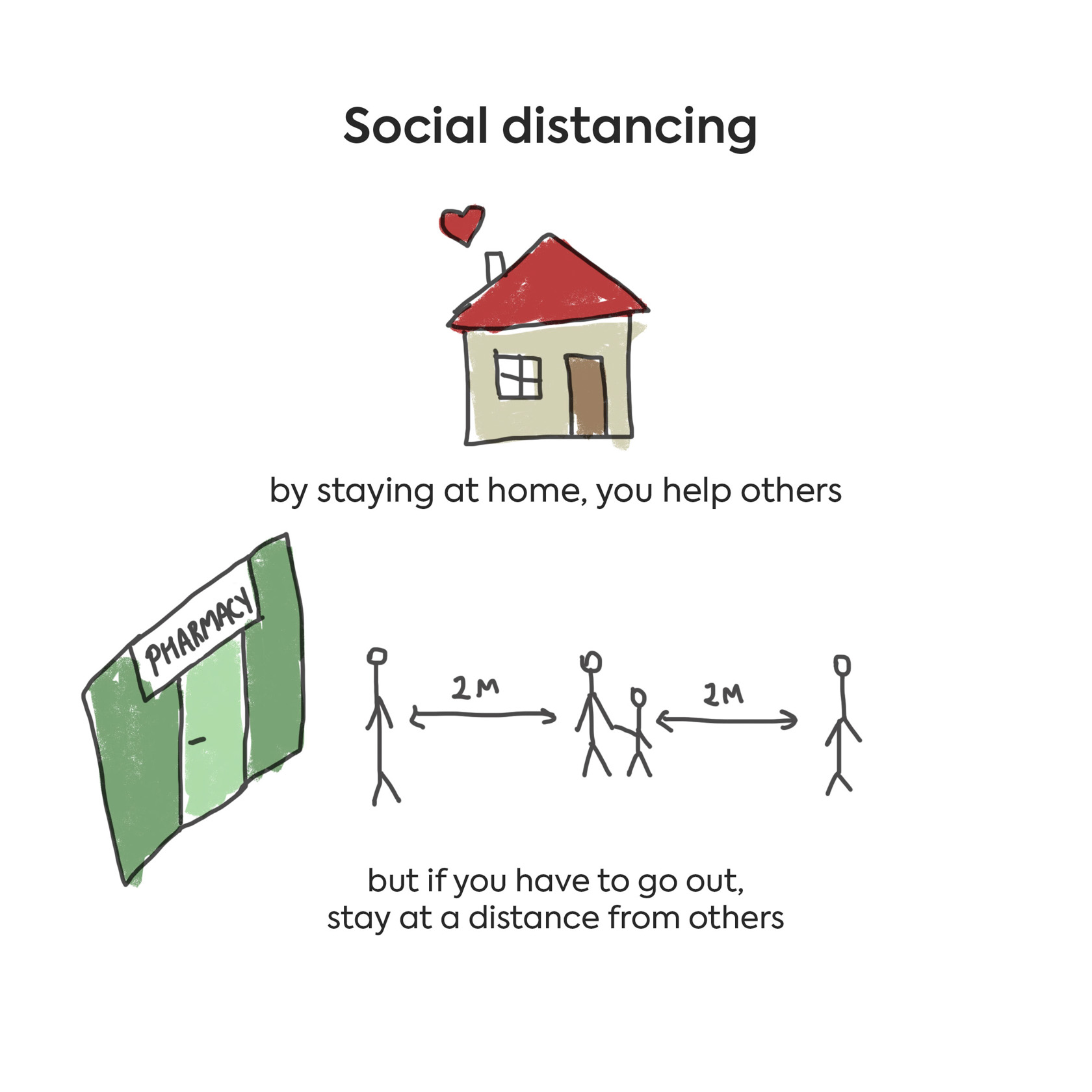
By staying at home, you reduce the possibility of transmitting the disease to others, including health workers who are needed to care for more seriously ill patients. By staying at home, you help others.
If you have symptoms of coronavirus, you need to stay home for 7 days after the onset of symptoms.
Before returning to your normal routine, at least 3 days should pass without a fever without the use of fever-reducing drugs. In addition, make sure you are not coughing or experiencing a sore throat. If you did not have a fever, stay home for at least 3 days after your symptoms pass.
If you live with someone who experiences symptoms, you will need to stay at home for 14 days from the day the first person in the house developed symptoms.
If you feel worse, experience shortness of breath, a higher fever, or an intensified cough, then urgently contact a doctor, call an ambulance, and go to the hospital.
If you live with a person who is 70 or older, who has a chronic illness, pregnancy or a weakened immune system (receiving treatment for cancer, HIV infection, immunosuppressants), try to find another place where they can live away from you for 14 days.
If you must stay at home together, try to stay as far apart as possible from each other (2 meters or three steps).
2. Rules for home quarantine upon the appearance of symptoms:
• Do not go to school or work
• Do not use public transport or ride in shared cars or taxis
• Isolate yourself as securely as possible from other people in your home.
• When you need to be near other people, wear a face mask
• Wash your hands often with soap and water for at least 20 seconds.
• Cover your mouth and nose with a tissue or your sleeve when you sneeze or cough. Throw away the tissue immediately and wash your hands.
• Clean frequently touched surfaces, such as countertops, doorknobs, bathroom fixtures, and telephones. Clean them after each use or at least once a day. Use a spray bottle with a household cleaner or cleaning wipes.
• Do not allow visitors to come to your home
If you live with a family, then family members must quarantine themselves for 2 weeks.
• Inside an apartment or house, it is advisable to stay at a maximum distance from each other. It’s better stay in separate rooms
• Use separate bathroom and toilets, if this is available
• If you use a shared bath or toilet, disinfect frequently touched surfaces after each visit.
• Avoid sharing personal household items, such as glasses, cups, cutlery, and towels
• Ventilate rooms frequently and clean with household cleaning products daily.
• Often (every day or every other day) change towels, bedding and underwear
How is the test for COVID-19 done?
Now, two tests are being done. The first is a rapid analysis of a nasopharyngeal smear; the second is a blood test. Both tests work by PCR (polymerase chain reaction).
The results of the rapid test become known in 1-2 days; the blood test takes longer (about 4-5 days), since the process takes place in several stages:
• Specialists from the central reference laboratory of the National Research Center for Highly Infectious Infections carry out laboratory diagnostics using PCR. The coronavirus’s ribonucleic acids (RNAs) are detected, which confirms coronavirus infection.
• In addition, all samples are tested for influenza, SARS, and other types of coronaviruses.
• All negative and positive patient samples are retested at the Virus Infections Laboratory of the National Center for Public Health of the Ministry of Health, accredited by the World Health Organization.
• Additional monitoring at a laboratory in collaboration with WHO.
The patient is kept in isolation in a medical institution during the entire testing process, supervised around the clock by specialists. The sample for analysis is taken by a medical professional. In all other cases, the analysis is not performed. Laboratories of private medical organizations do not conduct studies to detect new coronavirus infections.
If I get sick, does this mean that everyone I live with or am in contact with is sick?
Right now, it is believed that COVID-19 is a highly contagious infection. If a person falls ill with COVID-19, then there is a very high risk that family members and persons in close contact with that person might become infected. But to get an exact answer to this question, months or even years of observations and subsequent statistical processing of the data will be needed.
What treatment is currently offered to the infected?
At the outpatient level (if the patient is at home) there is no specific treatment. It is recommended to drink plenty of water, observe good hygiene and sanitation, and self-isolate so as to not infect other family members.
In the hospital, antiviral therapy (lopinavir/ritonavir) is prescribed, palliative care is provided and, if necessary, mechanical ventilation (life-support machines).
Are antibodies produced for COVID-19? Is it possible to get infected again?
To date, there is no conclusive answer to this question for the simple reason that this virus is new, and little is known about it. Cases of positive test results among patients who had already recovered from COVID-19 are indeed described in the literature. However, it is not yet clear whether they really became infected again after recovery, or whether these are test system errors. After all, both false positive and false negative test results are possible.
In addition, much depends on the characteristics of each individual’s immune system. According to the "rules", after an infection, protective antibodies circulate in the body for some time; these are able to immediately recognize and suppress the pathogen when they come into contact with it again. However, in order to find out how long these antibodies continue to remain in the body at a level sufficient to fight off disease, extensive observation is necessary.
How can we strengthen our immunity to prevent disease?
Proven methods of strengthening immunity include:
• Mindful, balanced nutrition
• Regular physical activity (at least 150 minutes of moderate and intense aerobic exercise per week; for example, walking at a fast pace, swimming or cycling)
• A good night’s sleep (at least 7-8 hours)
• Good personal hygiene
• Vaccinations
• Giving up bad habits (smoking, overuse of alcohol, drug abuse, etc.)
ANTISEPTICS AND DISINFECTION
Is any hand sanitizer suitable?
Alcohol-containing sanitizers kill viruses and bacteria best. Alcohol content should be at least 60-70%.
How do I wash my hands correctly?
Washing hands with soap following recommendations should take 30 seconds to 1 minute. Repeat each movement at least 5 times:
• Rub one palm against the other from the fingertips to the wrist
• Put the right palm on top of the back of the left hand. Place the fingers of the right hand in the spaces between the fingers of the left hand. Wash the back of the left hand with the right palm, then change hands
• Straighten your fingers, then twist them to rub the inner surfaces of fingers up and down
• Grasp your left thumb with your right hand and wash it with rotational movements; then, wash the thumb of the right hand with the left hand
• Grasp your left wrist with your right hand and wash it with rotational movements; then, wash your right wrist with your left hand
• Wash your left palm with the fingertips of the right hand in a circular motion; then, change hands
When you’re done, dry your hands with a paper towel, close the tap with it, and then throw the used towel into a garbage bin with a closing lid.
What is the best way to clean surfaces?
For cleaning home surfaces, use usual means for household cleaning, following the instructions on the packaging (to find out for which surfaces the product is intended, how to apply it, how to rinse it off, etc.).
Frequently clean surfaces such as tables, shelves, computer keyboards, door handles, toilet bowls, kitchen and writing tables, cabinet handles, telephones, TV remote controls, etc.
If you have bleach at home, you can make a disinfectant yourself: 60-100 ml of solution per 1 liter of water. When cleaning surfaces with any chemical agents, it is important to observe safety rules: wear gloves and make sure that the room is well ventilated.
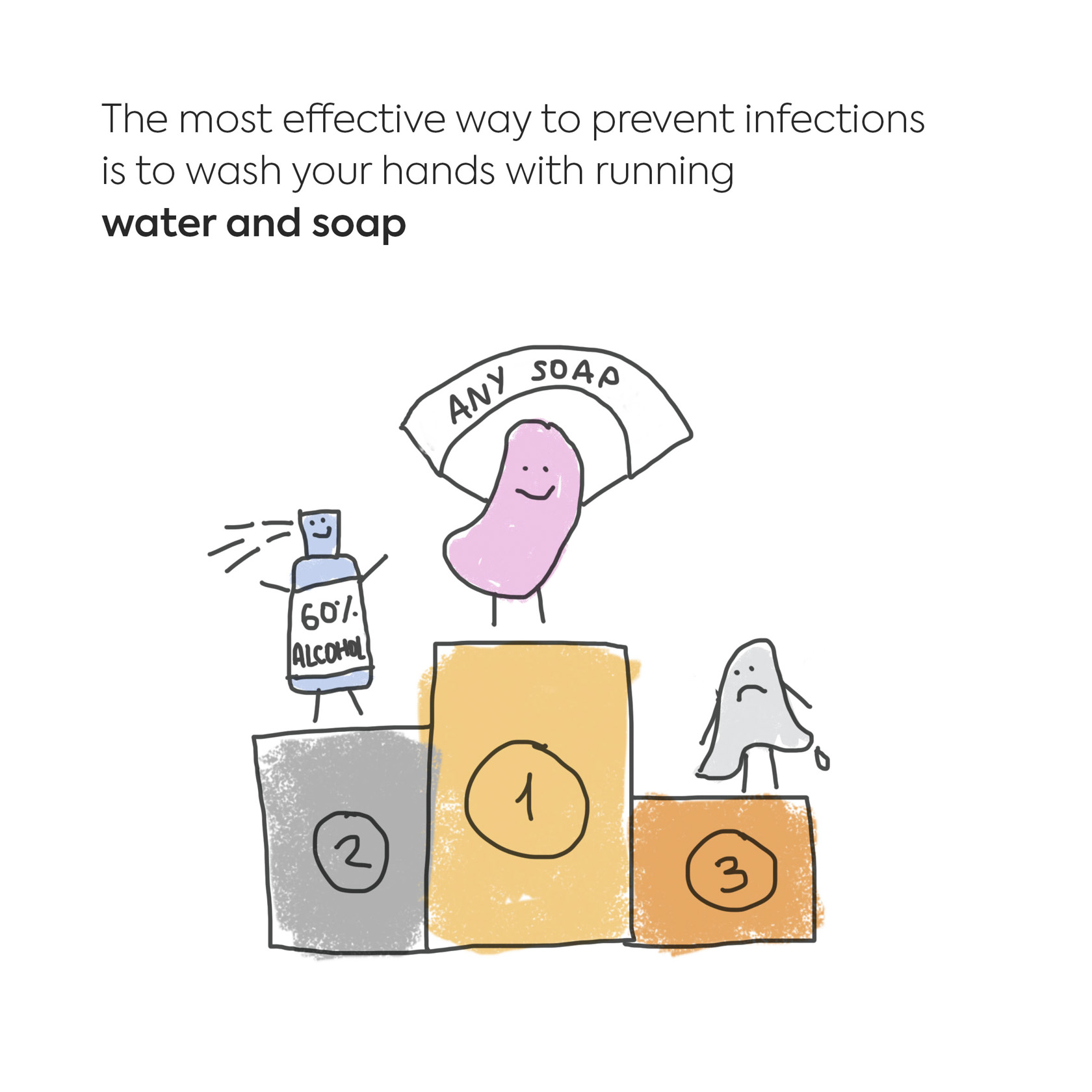
Do I have to wash my hands with antibacterial soap?
No, you can wash your hands with ordinary soap. The effect will be the same. Viruses are not bacteria, so antibacterial soap does not have any additional advantages compared to conventional soap.
Washing hands with soap and water allows you to wash away dirt, sweat, and grease from the surface of the hands to which viruses and bacteria stick. To achieve the best effect, you need to adhere to the guidelines for correct hand washing.
Which is better: sanitizer or antibacterial wipes?
The most effective way to prevent infections (viral and bacterial) is to wash your hands with running water and soap.
If there is no soap and water at hand, you can use alcohol-containing sanitizers (containing at least 60-95% alcohol).
Antibacterial wipes can reduce grime on the surface of the hands, but they are ineffective against viruses, as wipes rarely contain enough alcohol to kill them. Wipes are generally only effective against bacteria.
ANSWERS TO MYTHS AND ADVICE FROM SOCIAL NETWORKS
“Perhaps we all caught coronavirus last winter, so there’s nothing to worry about.”
This assumption has no scientific basis. COVID-19 is characterized by the fact that it occurs in mild to moderate form in the majority of the population, but it can rapidly lead to the development of severe pneumonia with acute respiratory failure or impaired renal function in people over 60 and in patients with chronic diseases of any age. Such patients need mechanical ventilation or even artificial blood circulation. This fact focused the attention of doctors, scientists and epidemiologists in China and around the world on this virus. And even though statistics tell us that only 15 to 20% of patients become seriously ill, when translated into absolute numbers, it becomes clear that no health system has sufficient resources to provide help to all those in need if it is inundated with many serious patients in a short period of time. If the virus had been present in our country since the winter, we, primary care doctors, ambulance services, and hospitals, would have been the first to know about it.
"A lot more people die from the flu every year."
In fact, it is incorrect to compare these two diseases. COVID-19 is considered a new disease until enough knowledge has been accumulated about what long-term health effects it can cause.
However, there is now evidence that even young people who have suffered from moderate to severe cases of COVID-19 can develop fibrosis in the lungs (proliferation of scar tissue), shortness of breath with the slightest exertion, and other symptoms of decreased lung function. These may persist until the end of life. That is to say, this disease may lead to early disability of young, able-bodied people. It is possible that after some time other previously unknown negative health effects of COVID-19 may be identified.
Therefore, comparing different viral infections with each other, focusing only on the number of deaths, is not entirely correct. Moreover, humanity has learned to protect itself from flu and reduce the number of deaths with the help of vaccines and antiviral drugs. Neither exists for COVID-19. Influenza mortality can be reduced by annual vaccinations, but unfortunately, to this day, not everyone understands the importance of vaccinations.
Tips from Taiwanese experts and Japanese doctors on diagnosis and prevention*
*Posts that have been widely shared on WhatsApp and other social media with health tips can contain incorrect information, such as:
- By the time a patient notices a fever or shortness or breath, 50% of their lung tissue already has fibrosis
- A person can check for fibrosis by holding their breath for 10 seconds. If they can accomplish this, they don't have fibrosis, and the conclusion is drawn that they don't have the infection, either.
- Taking a sip of water every 15 minutes can wash the virus from the nasal or throat cavity into the stomach, where stomach acid will kill it.
Below, doctors tell us the truths about these widely-circulated assumptions.
Regarding the incubation period with COVID-19: for now, everyone else should operate under the assumption that it is 14 days. This is maintained by the World Health Organization and all the leading centers in the world. The possibility of developing fibrosis in a mild case of coronavirus infection similar to SARS has been discussed but is not yet proven. Fibrosis occurs in less than 1% of patients, only after the infection has passed, and only in patients with severe cases who have experienced bilateral pneumonia, acute respiratory distress syndrome, prolonged mechanical ventilation and oxygenation.
The main symptom of fibrosis is shortness of breath and poor tolerance for physical exercise without the presence of a fever or other signs of pneumonia. The breath-holding test is a simple but unreliable test for exercise tolerance. Many people that don’t have fibrosis will still not be able to pass this test: those with heart failure, asthma, chronic obstructive pulmonary disease (COPD), and severe obesity, among others. All of these patients have compromised respiratory systems. The most reliable test for respiratory failure is to check how many steps a person can take in six minutes on a treadmill.
About water: everyone should drink 2 liters of pure water per day in addition to tea, coffee, compotes and other drinks. Wetting the mucous membranes of the mouth and throat with small sips of water is good advice for dry, hot weather or in dry rooms which result from heating in the winter months. The assertion that viruses can be washed from the oral cavity into the stomach where it will experience death by hydrochloric acid and pepsin is just a hypothetical assumption. There is no evidence. In addition, it must be remembered that the virus can also enter the body through the eyes and nose.

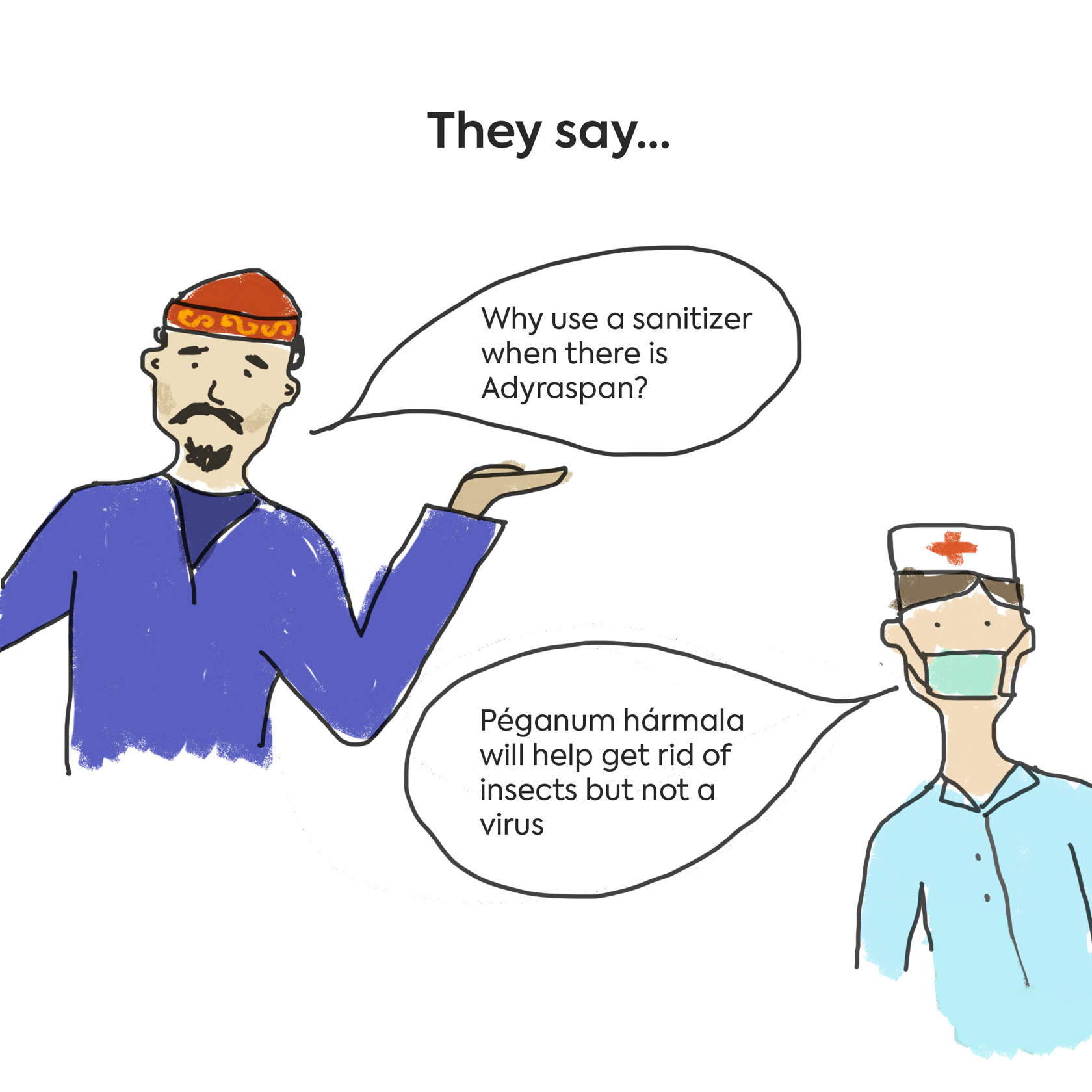
“Adyraspan and tail fat will protect me against coronavirus”
Refractory animal fats (tail fat, goose, etc.) create a film when rubbed onto the skin that slows down heat loss. Therefore, they have a warming effect that relaxes muscles, ligaments and relieves pain. Muscle pain often occurs along with a cold or infection, and such "physiotherapy" can provide relief of symptoms. But these fats do not cure any infection.
Adyraspan, or Péganum hármala, is a very effective insecticide that has been and is still used to fumigate rooms. You need to be careful if pregnant women occupy the room, because Garmala can cause premature birth or miscarriage. To date, the scientific community does not know anything about the antiviral properties of this herb, and there is no scientific evidence about whether the herb is effective against viruses and bacteria.
On March 16, the Association of Family Doctors of Kazakhstan launched a free online guide on issues related to the coronavirus infection COVID-19 on the official pages of ACVC on Facebook and Instagram for the population of Kazakhstan.
The Adamdar/CA team thanks the staff of the Association of Family Doctors of Kazakhstan and designer Aizhan Baitimbetova for their help in preparing the material.
Illustrations may only be used with the express written consent of Adamdar/CA.